What is plantar fasciitis and how can it be treated?
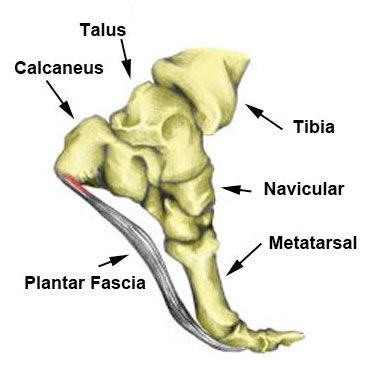
Plantar Fasciitis is a common injury of the foot with symptoms presenting as sharp or stabbing type pain in the plantar aspect (sole) of the foot, where the plantar aponeurosis inserts into the heel of the foot. It’s usually worst in the morning when getting out of bed, with the pain making it difficult to take the first few steps, then slowly improving as it warms up.
There are 2 main forms of plantar fasciitis;
- Acute onset plantar fasciitis is when the injury occurs suddenly – for example, landing heavily on a stone and injuring the soft tissue.
- Chronic plantar fasciitis is when the injury is caused by overuse, and leads to the development of micro-tears in the soft tissue. If not treated early, this can develop into a heel spur.
The Plantar Fascia is a fibrous band of connective tissue running from the anterior of the calcaneus (heel bone) to the base of the toes. It’s there to help maintain the integrity of the foot arch and act as a shock absorber when landing during running, jumping, etc. The plantar fascia is also active in the toe phase of running, walking, and jumping as it stores potential energy during the heel-off phase and releases kinetic energy during the toe-off phase.
Causes Of Plantar Fasciitis
OVERUSE INJURY (REPETITIVE STRESS) – sports such as running and dancing can place undue stress on the soft tissue on the plantar aspect of the foot over time. This is also true for people that are on their feet on hard surfaces for long periods of time.
EXCESS WEIGHT increases the risk of developing plantar fasciitis.
PREGNANCY weight gain, along with the release of relaxin (a hormone that relaxes the ligaments) will also increase the risk of plantar fasciitis.
FLAT FEET OR HIGH FOOT ARCHES – changes in the arch of your foot can affect the shock absorption ability and can stretch and strain the plantar fascia, which then has to absorb the additional force.
WEAK INTRINSIC MUSCLES are unable to support the foot, placing extra pressure on the plantar ligaments.
ARTHRITIS – some types of arthritis can cause inflammation in the tendons in the bottom of your foot, which may lead to plantar fasciitis.
DIABETES – plantar fasciitis occurs more often in people with diabetes, although doctors don’t know why.
POOR FOOT BIOMECHANICS play a large role in the onset of plantar fasciitis. For example, overpronation or stiff ankle joints often from a previous injury.
Preventing Plantar Fasciitis
- Wear correct footwear. Your shoes should be supportive and correct for your foot type and gait; this applies to work boots/shoes and athletic shoes equally.
- Have biomechanics and feet checked by a qualified practitioner, such as a Podiatrist or Myotherapist.
- Incorporate stretch and strengthen programs for the feet into a regular routine.
- Ice and massage the feet after a hard workout or long day of standing.
- Increase intensity and duration of exercise in small increments – no more than 10% per week.
Treatments For Plantar Fasciitis
REST & ICE TO REDUCE INFLAMMATION – either an ice pack or frozen drink bottle is suitable for this purpose. Rolling the affected foot over a frozen drink bottle will also massage the plantar fascia and assist with the pain-relief and healing process.
SOFT TISSUE MANIPULATION to relieve the plantar fascia and affected muscles and soft tissue supporting the foot.
TAPING to support the foot and reduce the load on the plantar fascia, allowing it to heal. Taping is also a useful diagnostic tool.
STRETCHING AND MOBILISATION EXERCISES to assist in loosening soft tissue to restore flexibility and ankle range of motion.
BIOMECHANICAL ASSESSMENT to correct any dysfunction, prevent future episodes, and determine the need for orthotics.
STRENGTHENING AND MOBILITY to strengthen the intrinsic and extrinsic muscles of the foot, taking pressure off the plantar fascia and restoring correct functionality of the foot.
NIGHT SPLINTS to keep the plantar fascia on stretch whilst sleeping, by keeping the foot in 5 degrees of dorsi flexion. Research has shown no definitive answer as to how effective night splints are, however along with other forms conservative treatment, they do assist in the healing process and help reduce symptoms.
Returning To Exercise:
It depends on the type and intensity of the injury, however you should be pain and symptom-free before full training is resumed, and you should build back to full training slowly at a rate of no more than 10% increase per week.